Editor’s Note: Lauren Ghazal, PhD, is a board-certified family nurse practitioner in New York and a postdoctoral research fellow at the University of Michigan in Ann Arbor. The views expressed here are her own. View more Opinion on CNN.
Ask any nurse in the United States – there are more than 4 million of us – “How are you doing?” and the answer will be the same: “Nurses are not OK.” After nearly two years, the Covid-19 pandemic has upended us.
I know this firsthand. I am a family nurse practitioner as well as a researcher. Over the past few months as Omicron cases have spiked, my colleagues and I have been stretched to our limits.

I see patients of all ages and from all walks of life, many of whom don’t have a primary care provider. I help them manage multiple aspects of Covid – testing, vaccination, treatment – in addition to filling in those gaps in primary care. Right now, there are no simple and quick health care visits, and there aren’t enough nurses to take care of the need. It has been heartbreaking to turn patients away because of the lack of available appointments.
But for many of the patients I treat, the reality of the pandemic today may feel better than it did in 2020. We have vaccines and booster shots, better treatment plans and a much more abundant supply of masks and other personal protective equipment (PPE). Much of the public, for better or worse, has found an equilibrium of living life while trying to mitigate the risk of contagion.
Inside the hospitals and clinics where I work, however, the reality is much different. For nurses, 2022 can often feel far grimmer than what we experienced at the start of the pandemic. We have vaccines and more PPE now, yes, but being on the front lines of waves of infections has carried an extreme physical and emotional burden that’s leading to immense burnout.
At times, I’ve received requests to pick up additional overtime shifts or to “volunteer” my time at a local hospital when other nurses have been out. When I get these requests, I feel a trepidation far worse than what I felt on that day in early April 2020 when an emergency alert popped up on my iPhone, “Attention all healthcare workers: New York City is seeking licensed healthcare workers to support healthcare facilities in need.” When I read those words, I knew we were in crisis. What I didn’t know is the extent to which our workforce would suffer.
It is more than the labor of taking care of a greater number of patients that is wearying. It is also the hopelessness that comes from seeing no end in sight and meeting people who won’t face the truth. I encounter vocal fellow Americans who still deny that the pandemic is a real threat, that the SARS-CoV2 virus that causes Covid-19 is airborne, that people can die from it (currently more than 5.5 million globally) or suffer from long-term complications. This rejection of reality feels like betrayal.
While my colleagues and I are doing everything we can to treat patients despite our own exhaustion, there are still patients filling waiting rooms who have not gotten vaccinated or taken preventive measures such as wearing masks to protect themselves and help curb the influx of new Covid-19 hospitalizations. And while some of the public may choose to be “done” with the pandemic, or live as though it doesn’t exist, for health care workers like myself there has been no escape.
So, now when I get a request to pick up extra hours due to staff shortages, I am faced with a dilemma: take on the work and add to my already considerable exhaustion or turn it down and know that patients and the stretched-thin nursing staff will suffer as a result. Many times, I choose to take on the work.
My friends and colleagues in the nursing profession have said that they face the same tug of war between taking care of themselves and taking care of others. “If I don’t show up, who will? We don’t have enough nurses to safely care for our patients,” one colleague told me. Our burnout is caused by a systemic mess we didn’t create but one that we are forced to address daily.
The pandemic has broken open the cascade of problems leading to this health care emergency in nursing. We don’t have enough skilled nurses to treat the number of patients across all health care settings. On top of that, we have a pipeline issue: To train more nurses, we need more educators, but universities are struggling to fill faculty backlogs because, sadly, nurse faculty salaries are far lower (on average $20,000 less) than clinical or private sector roles.
Without financial boosts to nursing schools, expanding loan forgiveness for nurse educators and researchers, and funding of the Department of Health and Human Services’ Medicare Graduate Nurse Education Demonstration, nursing schools may continue to face faculty shortages. Additionally, the American workforce is undergoing a rapid transformation as part of the “Great Resignation,” as American workers seek a better work-life balance than the generations before us.
For nurses, that means turning toward options like travel nursing – short-term employment contracts in hospitals and regions that are in dire need but that also offer compensation that easily eclipses the salary of local staff nurses. These types of assignments are not new, but they’re now in high demand, creating a precarious impact on the financial health of hospitals.
Each day, I am tempted by the emails I receive from travel nurse recruiters for both registered nurse and nurse practitioner positions. And I know I am not alone when asking: Why should nurses tolerate the exceedingly high workloads and verbal and physical abuse without the higher pay that travel nursing assignments offer? Especially given that inadequate compensation is a contributing factor to nurse burnout.
Earlier in the pandemic, there were brief glimpses of light. I remember the overwhelming emotion I felt while receiving my first Moderna vaccination as a cancer survivor and frontline worker at a New York Department of Health building in Harlem in early January 2021. And for a while, scrolling on social media, I would find a friend or family member post proudly about receiving a vaccine. Speaking to other nursing friends who were working in intensive care units, there was also a shift to better treatment plans for Covid-19. While we were exhausted, we were hopeful.
Now, as we enter our third year of the pandemic, those helpful feelings are hard to hold onto. Many nurses are left to silently suffer as they face overwhelming feelings of exhaustion, irritability, anxiety and sadness that are chipping away daily at our mental health. One recent study published in JAMA Psychiatry found that, compared to the general female population, female nurses are at two times higher risk of death by suicide.
This raises the question: In a pervasive pandemic with the potential for continued infection and illness, can the United States afford to ignore nurse suffering? Neighbors have performatively applauded nurses for our resiliency, yet our leaders have failed to provide critical support to nurses that moves beyond the performance.
Providing mandated nurse staffing to ensure patients can continue to receive high quality of care, offering higher compensation and providing mental health support are three places to start. More direct, a January 20 letter from the Massachusetts Nurses Association to Gov. Charlie Baker explicitly details 14 steps that he and hospital administrators should take to address this health care crisis in nursing.
Earlier this year, the nursing profession was once again ranked highest in honesty and ethics – an honor it has touted for 20 years. But now, this honest and ethical profession is shrouded in extreme burnout. The human and emotional toll that nurses have been asked to shoulder has come to a head, and we need your help. We ask the public to mask up, vaccinate and stay home if you have symptoms or test positive. And we ask for more leaders, inside and outside the nursing field, to advocate for higher wages and nurse faculty packages.
Nurses have long been advocates for our patients, and now we need both patients and employers to value our lives and labor and advocate for us. Let us all practice some compassion and patience, not only for our nurses and health care workers but for each other. At this rate, our workforce will continue to crumble if bold changes aren’t made.
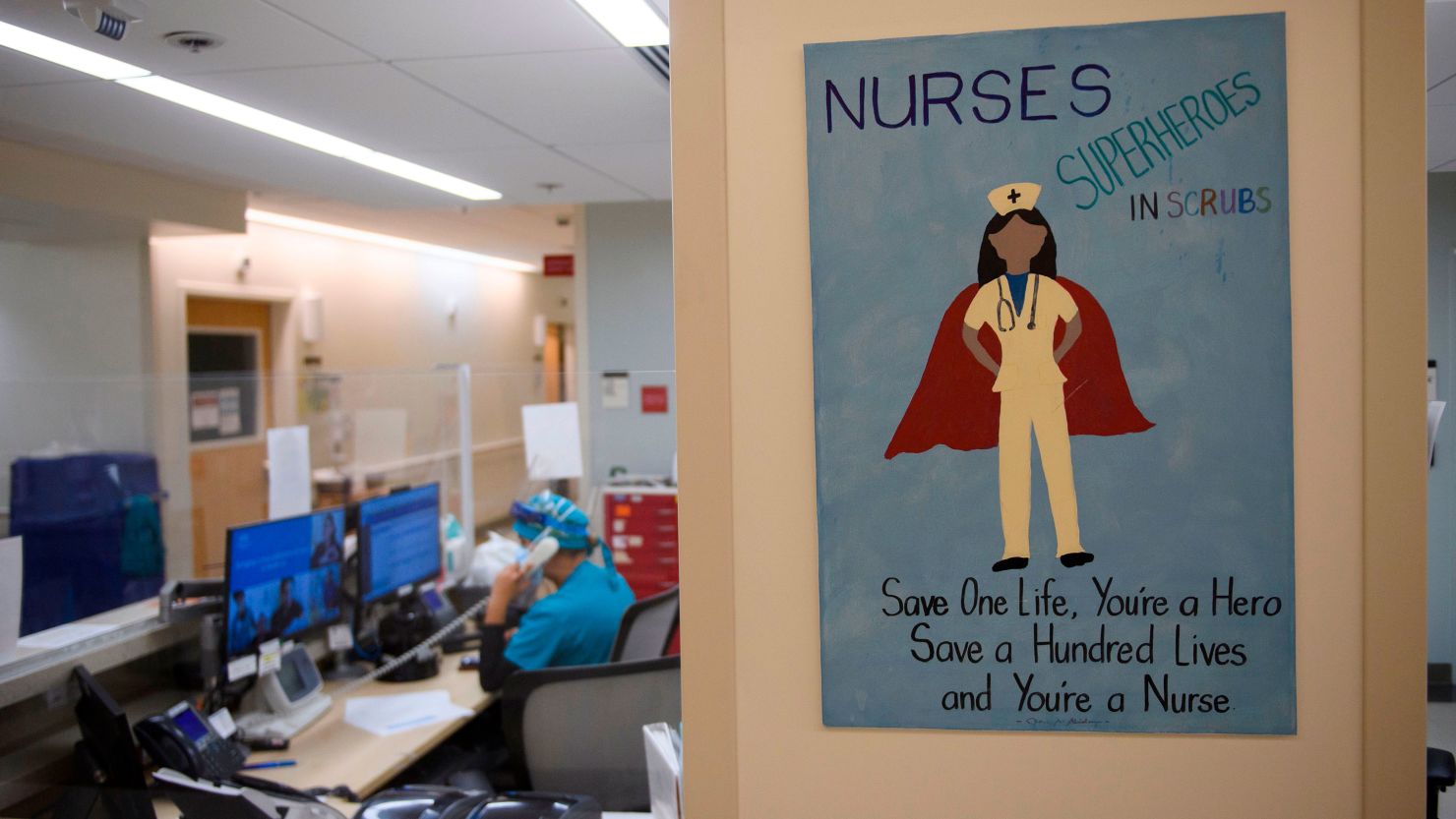
Since the start of the pandemic, nurses and other frontline workers have been called heroes. I often balk at the hero title; it perpetuates the idea that nurses’ self-sacrifice is acceptable and no help is needed. But in fact, we do need help, and we need it quickly.