Watch CNN’s “Coronavirus Town Hall: The Vaccines,” hosted by Anderson Cooper and Dr. Sanjay Gupta, at 9 p.m. ET/6 p.m. PT Friday.
The vote to recommend long-term care residents be among the first to receive Covid-19 vaccinations was not unanimous.
Out of a panel of 14 CDC vaccine advisers, a lone doctor said no.
“Odd woman out, I guess,” Dr. Helen “Keipp” Talbot, of Vanderbilt University, told her colleagues. “I still struggle with this. This was not an easy vote.”
Talbot was worried about whether the vaccine would even work in such frail, vulnerable patients. Even more, she worried about how it might look if the vaccine failed in that group, or how it would affect public perception if residents died soon after getting the vaccine.
On the other hand, these are the people worst hit by the pandemic. They make up 40% of all deaths so far.
Nursing homes in the Midwest have been particularly hard hit, with a more than 400% increase in weekly cases since mid-September, according to a report published Tuesday by the American Health Care Association and National Center for Assisted Living. During the week of November 15, 49% of new nursing home cases were in the Midwest.
Between mid-September and the week of November 15, there was a 177% rise in new weekly nursing home cases nationwide. The rise in cases has been accompanied by a rise in coronavirus deaths in nursing homes.
“Our worst fears have come true as Covid runs rampant among the general population, and long term care facilities are powerless to fully prevent it from entering due to its asymptomatic and pre-symptomatic spread,” said Mark Parkinson, the organization’s president and CEO.
Simpler logistics
From a practical standpoint the reason to vaccinate is simple.
It is much easier to send a team to a facility and vaccinate everyone who works and lives there at the same time than it is to vaccinate the two groups at different times. Since the vaccine requires two doses, the vaccinators already have to return about 21 days later as it is.
“That’s two trips versus four trips, at a minimum,” said Dr. Kelly Moore, associate director of the Immunization Action Coalition, which is supporting frontline workers who will administer Covid-19 vaccinations.
“From a practical standpoint of how quickly can we get people vaccinated who need it, it simply simplifies the logistics drastically because people in long-term care can’t actually go to a vaccination place. You have to bring the vaccine to them. And so it’s much easier if we can vaccinate everyone who needs it on one trip, instead of having to make multiple trips at different times to the same facility over and over.”
From a medical standpoint the reason to vaccinate long-term care residents is more complex.
They are the group of Covid-19 patients with the highest mortality rate, and many of the hospitalizations are people who are from long-term care facilities who contract Covid-19 and are hospitalized. When they get sick, it generates a lot of burden on hospitals.
“Those are all very good reasons to vaccinate the residents,” Moore said.
But there is also reason for concern. The Covid-19 vaccines have not been tested in the frail elderly, many of whom are residents of long-term care facilities.
“Since they haven’t been studied in people in those populations, we don’t know how well the vaccine will work for them. We know that most vaccines don’t work nearly as well in a frail elderly person as they would in someone who is fit and vigorous, even if they happen to be the same age,” Moore said.
“There’s a question about the direct benefit of the vaccine, if given to people who live in those facilities, because we haven’t studied how well it works in that group yet.”
It’s this uncertainty that led Talbot to vote no.
“I have spent my career studying vaccines in older adults. And we have traditionally tried a vaccine in a young healthy population and then hoped it works in our frail older adults,” she told the committee ahead of her vote. “And so we enter this realm of ‘we hope it works, and we hope it’s safe,’ and that concerns me on many levels.”
When shots begin to go into arms of residents, Moore said Americans need to understand that deaths may occur that won’t necessarily have anything to do with the vaccine.
“We would not at all be surprised to see, coincidentally, vaccination happening and then having someone pass away a short time after they receive a vaccine, not because it has anything to do with the vaccination but just because that’s the place where people at the end of their lives reside,” Moore said.
“One of the things we want to make sure people understand is that they should not be unnecessarily alarmed if there are reports, once we start vaccinating, of someone or multiple people dying within a day or two of their vaccination who are residents of a long-term care facility. That would be something we would expect, as a normal occurrence, because people die frequently in nursing homes.”
On Tuesday, the American Health Care Association and the National Center for Assisted Living applauded the CDC advisory committee’s 13-1 vote to recommend prioritizing their residents.
“More than 100,000 long term care residents have died from this virus in the U.S. and our nursing homes are now experiencing the worst outbreak of new cases since last spring with more than 2,000 residents succumbing to this virus each week,” said Parkinson. “We are extremely hopeful this vaccine will literally be a lifesaver for thousands of residents.”
Some state governors have begun to indicate that they will follow the CDC’s priorities for distributing the vaccine to both healthcare workers and long-term residents.
In Georgia, more than 95% of nursing homes in the state have enrolled with the CDC through partnerships with CVS and Walgreens for vaccine rollout and distribution.
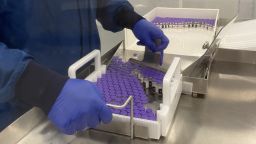
Nationwide, CVS is preparing to administer Covid-19 vaccinations to approximately 2 million long-term care facility residents, according to Chris Cox, senior vice president of CVS Health. Walgreens is preparing to administer the vaccine to approximately 1 million long-term care facility residents, according to Rick Gates, senior vice president of pharmacy and healthcare at Walgreens.
The pharmacy chains plan to store the vaccine at approximately 1,900 “hubs” across the country and then distribute it to more than 48,000 long-term care facilities nationwide.
CVS chief medical officer Dr. Troy Brennan, told CNN’s Kate Bolduan on Thursday their plan is to be ready to go as early as December 15.
“We’re working with each of the states now, and it will be challenging because each state will be different,” Brennan said. “Some states will say just vaccinate the people in the skilled nursing facility. Some states will want us to vaccinate not only the people in the skilled nursing facility but the healthcare workers in those facilities, so those kinds of details are going to vary from state to state.”
Ending the isolation
The debate on whether to vaccinate residents of long-term care facilities, and the planning to get the vaccinations done, has occurred as the residents themselves have been largely isolated from family and friends in facilities that have been closed to visitors.
In addition to saving lives, Parkinson said he hopes the vaccine will “expedite the reopening of our facilities to family members and loved ones.”
But when that will happen remains unknown.
“The most pressing issue at the moment is ensuring that all long term care staff and residents are the first priority for a vaccine. Long term care facilities will not be able to have any sense of normalcy until a vaccine is administered, and we know that everyone is eager for that to happen,” said Cristina Crawford, a spokesperson for the American Health Care Association, in an email to CNN. “We hope to be able to discuss what next steps look like once a vaccine is being delivered and administered to staff and residents across the country.”
Moore said not to expect a change in policy out of the gate.
Get CNN Health's weekly newsletter
Sign up here to get The Results Are In with Dr. Sanjay Gupta every Tuesday from the CNN Health team.
“Right now, we just don’t have the data to know how well the vaccines will work in these folks, and so we’re going to need to be cautious at first because we know they are by far the most vulnerable to severe illness and death from Covid. We’re going to play it really carefully until we know for sure that these vaccines will really be effective at protecting them,” Moore said.
“As we learn more and we see if the vaccine works really well in these groups, then certainly my hope is that we can help these folks reconnect with their families because they need each other.”