Story highlights
- Experts call STDs in America "a public health crisis"
- A record number of STD cases were diagnosed in the US in 2017, according to preliminary CDC data
(CNN)Rates of syphilis, gonorrhea and chlamydia have climbed for the fourth consecutive year in the United States, the Centers for Disease Control and Prevention announced Tuesday at the National STD Prevention Conference in Washington.
Last year, nearly 2.3 million US cases of these sexually transmitted diseases were diagnosed, according to preliminary data.
That's the highest number ever reported nationwide, breaking the record set in 2016 by more than 200,000 cases, according to the CDC.
"It is time that President Trump and [Health and Human Services] Secretary [Alex] Azar declare STDs in America a public health crisis," David Harvey, executive director of the National Coalition of STD Directors, which co-hosted the conference said Tuesday.
"What goes along with that is emergency access to public health funding to make a dent in these STD rates and to bring these rates down and to ensure that all Americans get access to the health care that they need," he said.
Rob Stephenson, a professor and director of the Center for Sexuality and Health Disparities at the University of Michigan in Ann Arbor, said that "it's not a surprising trend."
"I think over the last five years, we've seen a rapid increase in the prevalence of sexually transmitted infections in the US, and we're also starting to see a plateau in our fight against the HIV epidemic, as well," said Stephenson, who was not involved in the new CDC research.
In 2013, there were 1,752,285 total cases of chlamydia, gonorrhea and syphilis diagnosed in the United States. That number grew to 1,811,850 in 2014; 1,945,746 in 2015; 2,094,682 in 2016; and 2,294,821 in 2017, according to the preliminary CDC data.
"We're talking about millions of infections with just these three infections," said Dr. Edward Hook, endowed professor of infectious disease translational research at the University of Alabama at Birmingham's School of Medicine and scientific committee chair of the National STD Prevention Conference.
It's concerning to see such tremendous and significant increases in STD rates across the country, Hook said.
"Gonorrhea diagnoses that were reported to the CDC increased by nearly 67%. Diagnoses of primary and secondary syphilis increased over 75%, and chlamydia rates continued to increase," he said. "It's important to remember that while these are preliminary data, and the data are eight months out of date. There's absolutely no reason to think that the increases that are being described by the CDC haven't continued into 2018."
Chlamydia, syphilis, gonorrhea
The preliminary data suggest that more than 1.7 million cases of chlamydia were diagnosed in 2017, with about 45% -- 771,340 cases -- emerging among 15- to 24-year-old women and girls.
Chlamydia, which remained the most common STD reported to the CDC, is caused by the bacterium Chlamydia trachomatis and easily transmitted during any form of sexual activity. If not treated, chlamydia can lead to pelvic inflammatory disease in women, which can cause permanent damage to the reproductive system. In men, the infection can spread to the tube that carries sperm from the testicles, causing pain and fever.
Meanwhile, syphilis diagnoses jumped from 27,814 cases in 2016 to 30,644 in 2017, according to the preliminary data. Men who engage in sexual activity with men made up 17,736 of those syphilis cases in 2017, the data suggest.
Syphilis, caused by the bacterium Treponema pallidum, can affect the heart, nervous system and other organs if left untreated. Syphilis is most often transmitted through sexual contact, although it also can be transmitted in other ways, such as from mother to baby, which is called congenital syphilis.
"We know today that some of what is driving congenital syphilis are women who are trading sex for drugs and that that explains some of the infections we are seeing in babies of syphilis," Harvey said Tuesday.
"There are infectious disease consequences of the opioid epidemic in America, including sexually transmitted infections," he said.
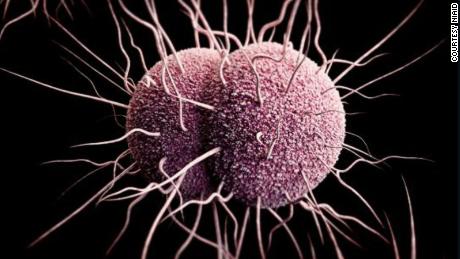
Gonorrhea diagnoses increased from 468,514 in 2016 to 555,608 cases in 2017, according to the data. Among men only, cases climbed from 270,033 in 2016 to 322,169 in 2017, the data suggest.
If not treated, gonorrhea can cause severe and permanent health issues, including problems with the prostate and testicles in men or problems with pregnancy and infertility in women.
Gonorrhea is typically treated with a dual therapy of the antibiotics ceftriaxone and azithromycin.
Yet the threat of antibiotic-resistant gonorrhea persists nationwide.
'We are sliding backward'
"Over the years, gonorrhea has become resistant to nearly every class of antibiotic we've used to treat it, except for ceftriaxone. The only remaining highly effective antibiotic to treat gonorrhea in the United States now," Dr. Gail Bolan, director of the CDC's Division of STD Prevention, said Tuesday.
In other words, though there have been a few documented cases, widespread resistance to ceftriaxone has not been seen.
There was a recent report of a ceftriaxone-resistant Neisseria gonorrhoeae isolate in a patient in Canada. As of October 2017, "only (five) ceftriaxone-resistant Neisseria gonorrhoeae isolates had been reported worldwide," according to a report published in the CDC journal Emerging Infectious Diseases in February.
In England, a man was infected with a form of gonorrhea that was resistant to the first-line treatment, a combination of the antibiotics azithromycin and ceftriaxone. Public Health England reported that case in March. The man was treated intravenously with the antibiotic ertapenem.
"Since 2015, CDC has recommended health care providers prescribe a combination of two drugs to people diagnosed with gonorrhea, a single shot of ceftriaxone and an oral dose of azithromycin," Bolan said.
"That approach seems to be working," she said. "Emerging resistance to ceftriazone has not been seen since the dual therapy approach was implemented, and there has not yet been a confirmed treatment failure in the United States when using the recommended therapy."
If gonorrhea becomes resistant to all such combinations of antibiotic therapies, it could become an untreatable STD.
Overall, "it's important to realize that the gonococcus, the bacteria that causes gonorrhea, has reliably developed resistance to every antibiotic that has ever been used to treat the infection. But in the past 15 to 20 years, the number of new antibiotics available and the development of new antibiotics has slowed greatly," Hook said.
"So we have this continued inexorable process of the gonococcus developing antimicrobial resistance, coupled with fewer new antibiotics to pick up and take care of the problem if it develops," he said. "That's a very troublesome combination."
CDC's preliminary data show that emerging resistance to azithromycin is on the rise in laboratory testing. In 2013, 1% of gonorrhea samples showed emerging resistance to the drug, but that number had risen to more than 4% in 2017, according to the CDC.
All in all, "we are sliding backward," Dr. Jonathan Mermin, director of the CDC's National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said in a news release about the new numbers of reported cases.
"It is evident the systems that identify, treat, and ultimately prevent STDs are strained to near-breaking point," he said.
The National STD Prevention Conference, where the preliminary data were presented, continues until Thursday. During the program, health care professionals, scientists and other experts will discuss the STD epidemic and possible solutions.
Why STD rates are rising, and how you can stay safe
Hook noted that such solutions could include increasing STD testing and treatment services, as well as increasing funding for health clinics and surveillance programs.
"It's important for the public to understand that most sexually transmitted infections are transmitted by people who do not know that they're infected," he said.
"We need to encourage health care professionals to routinely test and evaluate their patients for sexually transmitted infections," Hook said. "For every sexually active woman in the United States under age 26, it's recommended that those women get tested for Chlamydia trachomatis, the most common sexually transmitted infection in our country, every year -- and yet current data are that that happens for less than half of women."
The University of Michigan's Stephenson said that prevention is key to reducing the number of new STD cases -- such as practicing safe sex and getting tested regularly.
"Yet I think, when we think about sexually transmitted infections, we think of them through a curative lens, not a preventative lens," Stephenson said.
"We need to switch the dial on this in people's minds to think more about prevention rather than a too-late curative response," he said. "There's many ways we could do this. We could teach primary care providers and physicians to talk more about prevention with a client. We could start very early on in sex education by talking about the prevention of sexually transmitted diseases at young ages by giving people the behavioral skills they need to protect themselves."
At the same time, there have been declining resources for the CDC's Division of STD Prevention, Hook said.
"The purchasing power of the CDC's budget for sexually transmitted disease prevention has declined 40% in the past 15 years," he said. "The CDC and the public health clinics, where most of this reporting comes from, represent the safety net for Americans, for people who may not have access to primary care providers or other sources of care. So the decline and the limited availability of resources for that is no doubt part of the contributor."
Get CNN Health's weekly newsletter
Sign up here to get The Results Are In with Dr. Sanjay Gupta every Tuesday from the CNN Health team.
In recent years, state and local STD programs have seen budget cuts, too. In 2012, 52% of such programs experienced budget cuts, amounting to reductions in clinic hours, contact tracing and screening for common STDs, according to the CDC.
Additionally, the direct medical costs of treating STDs in the US are not cheap.
The 19.7 million cases of sexually transmitted infections that occurred in 2008 in the US equaled about $15.6 billion in total lifetime direct medical costs, according to a study published in the journal Sexually Transmitted Diseases in 2013.
"I do think we've seen significant funding cuts in prevention efforts around sexual health in general," Stephenson said. "It's not a difficult jump to see how that's actually preventing us from winning the fight against negative sexual health outcomes."