Story highlights
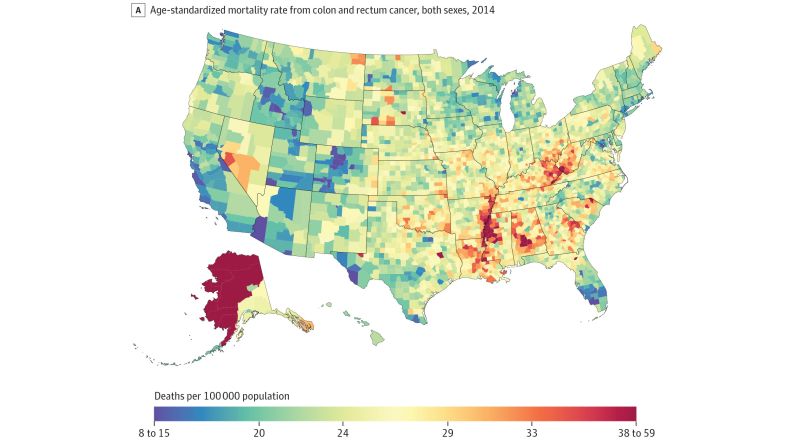
Colon and rectal cancer rates are rising for adults under 55, but the reason is unclear
Experts think this is unlikely to lead to major changes in screening recommendations
Colon and rectal cancer rates are rising sharply for Americans under 55, according to a study published today.
Someone born in 1990 would have twice the risk of colon cancer and four times the risk of rectal cancer at the same age had they been born in 1950, according to researchers at the American Cancer Society and the National Cancer Institute.
Because routine screening is generally not recommended for most people under 50, these cancers are often found in more advanced stages, too.
“What we found was pretty surprising,” said Rebecca Siegel, an epidemiologist at the American Cancer Society and the lead author of the study.
Siegel added that the surge of younger diagnoses contrasts with the overall trend of colorectal cancer, which has been dropping for several decades. However, this progress is driven by older adults who have benefited from regular screenings, including colonoscopies, that may pick up growths before they become cancerous, she said.
Siegel also said that the data – which looked at nearly 500,000 cases of colorectal cancer from 1974 to 2013 – do not reveal the reasons behind the increase.
“That’s the billion- or trillion-dollar question,” said Dr. George J. Chang, chief of colorectal surgery at MD Anderson Cancer Center. “Boy, it would be great if we knew.”
Two years ago, Chang made a statistical prediction using the same data: By 2030, roughly one in 10 colon cancers and one in four rectal cancers will be diagnosed in people under 50, the recommended screening age.
“It’s really important to highlight this issue because … young individuals ignore some of the symptoms, and they don’t get worked up,” Chang said.
Not leveling off
“I wouldn’t make too much of this,” said Dr. H. Gilbert Welch, a professor at the Dartmouth Institute for Health Policy and Clinical Practice.
The numbers, Welch said, are too small to warrant the attention this trend is getting.
Over three decades, the annual rate of colorectal cancer for folks in their 20s increased from one to two cases for every 200,000 people, according to Siegel’s study. For all adults under 50, the rate of colorectal cancer in 2013 was just over seven cases per 100,000 people.
Meanwhile, for those 50 and up, colorectal cancer rates have dropped over 100 cases per 100,000 people: from 226 in 1985 to 117 in 2013.
“More importantly,” Welch said, “there is no corresponding change in mortality” for younger adults.
Just because cancer rates are rising among younger adults does not mean they are dying at higher rates, according to Welch.
“The good news is that it’s still uncommon in individuals under 50,” Chang agreed, but it’s really the speed of the rise that concerns him.
“It’s important for us to be thinking about this, because it’s clearly not a trend that seems to be leveling off,” he said.
An uncertain future
Allison Rosen, a cancer prevention advocate in Houston, was not thinking about numbers and statistics when her doctor asked her to discuss the results of her colonoscopy in person.
“I knew right then that it was colon cancer,” said Rosen, who was 32 when she was diagnosed.
Rosen – who has Crohn’s disease, a risk factor for colon cancer – said she probably sought care earlier than other young people because she was “in tune with (her) body.” Even then, she put off her colonoscopy while her symptoms worsened.
“I just had the worst cramps I’ve ever had in my life,” said Rosen, now 36.
Other common symptoms include bloating, weight loss, constipation and blood in the stool, which can often be mistaken for hemorrhoids.
Siegel, the study author, said she knows of young patients who waited much longer than Rosen.
“I’ve heard stories of young people having symptoms for literally years,” she said.
Siegel added that young people are more likely to be uninsured, which can lead them to avoid seeing a doctor until they can’t ignore their symptoms any longer.
“That’s sort of a hot-button issue right now,” she said. “We had such great strides just in the past few years in insurance coverage because of the Affordable Care Act.”
Siegel said that the Affordable Care Act has been associated with cancers diagnosed at earlier, more treatable stages, which has been supported by a body of research.
“We know that this translates into real progress,” she said.
Harms and benefits
Though no one knows exactly why colorectal cancers are increasing among the younger age groups, researchers say it’s probably not driven primarily by our genes.
“It would be hard to speculate that we are fundamentally so different genetically between 1950 and today,” Chang said. “What’s really changed more are our environmental exposures, our lifestyles and our behaviors.”
Siegel said the rise of obesity, for example, has closely mirrored the trends in colorectal cancer. Obesity may not be a direct cause of colorectal cancer, Siegel said, though it may share common risks – such as sedentary lifestyles and unhealthy diets.
If obesity were the primary cause, Siegel said, “you wouldn’t expect to see (an increase in colorectal cancer) for 10 or 20 years.”
A 2014 study showed a 10% increased risk for colon cancer for each five-point increase in body mass index – which may be the difference between what is considered normal and overweight.
The American Cancer Society is reviewing colorectal cancer screening guidelines, a representative confirmed.
But physicians Siegel, Chang and Welch do not think that a major change in screening guidelines is imminent without more research.
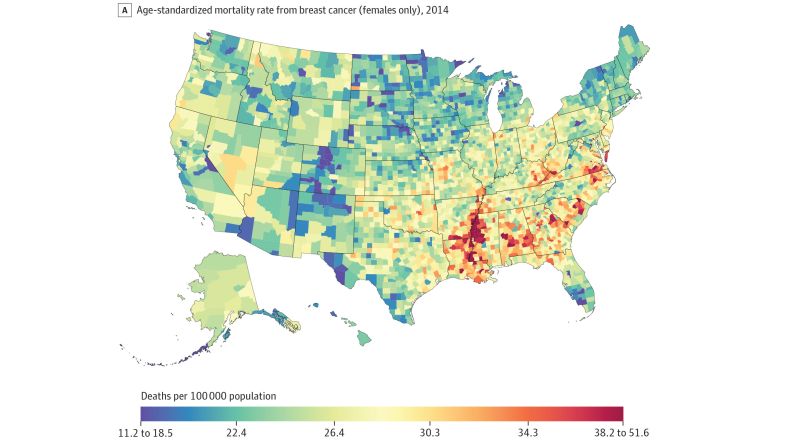
Colonoscopies and other screening tests come with “both harms and benefits,” Chang said. He compared the possibility of broader colorectal screening to the controversy surrounding mammograms – which have been shown to prevent breast cancer but may also lead to unnecessary and potentially harmful biopsies and treatments.
Chang thinks advances in less-invasive tests could change that conversation. For example, the Cologuard stool test, which was FDA approved in 2014, can be taken at home but is better at detecting growths that have already become cancerous.
Until then, he said, one measure may be more important that reconsidering screening guidelines: raising awareness among patients who may ignore their symptoms and among doctors who might not consider cancer in their younger patients.
Follow CNN Health on Facebook and Twitter
That is where cancer advocate Rosen has dedicated her career.
“Who would’ve thought that going through cancer would’ve helped me figure out want I wanted to do with the rest of my life?” she said.
“The more (awareness) we have, the more young adults will see it and think about what’s going on with them – and hopefully get screened,” she said.