Story highlights
- A 13-year-old died Friday as a result of an allergic reaction
- She received three injections of epinephrine, often a life-saving medication
- More and more children are finding out that they have food allergies
Friday was the last day of vacation for Natalie Giorgi. The 13-year-old took a bite of a dessert at the summer camp where her family was staying, but spit it out because something didn't seem right.
Later that evening, she was pronounced dead.
Natalie died of a severe allergic reaction to peanut butter, CNN affiliate KXTV reported. Her sudden death in California is especially alarming for the food allergy community because, according to a family friend's account to KXTV, Natalie received three epinephrine injections. Epinephrine is the only treatment known to prevent a serious allergic reaction from turning deadly.
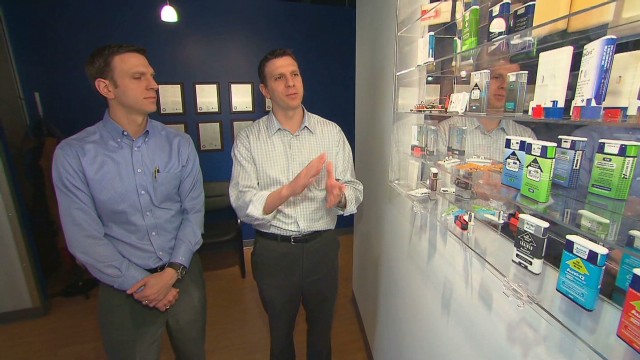
Anyone familiar with food allergies knows how important epinephrine auto-injectors are in emergency situations. Allergists recommend having multiple epinephrine auto-injectors available at all times for people with a risk of anaphylaxis.
Anaphylaxis symptoms include difficulty breathing, swelling of the throat or tongue, rapid pulse, nausea and vomiting. Allergies to medications, latex and insect venom, in addition to foods, can make the body go into shock in this way.
In general, a fatality is very unlikely if someone who's having a serious allergic reaction receives the appropriate dose of epinephrine quickly, said Dr. Clifford Bassett, director of Allergy & Asthma Care of New York, who did not treat Natalie.
"Any time we hear something like this, it's such a tragedy, because we all think in the allergy community that this stuff is preventable, treatable and so forth," he said. "And the answer is, there is no 100% in life."
Research has found that the effectiveness of epinephrine can be diminished if there is a delay in administering it, if an insufficient dose is given or if the medication has expired. More details of what happened to Natalie would need to be disclosed in order to make a definitive statement in her case, Bassett said.
Up to 40% of people need a second or third dose of epinephrine during a severe allergic reaction, he said, noting that it needs to be given in a timely fashion. After receiving a shot from an epinephrine auto-injector, the patient should get follow-up emergency care immediately.
Food allergies increased 18% between 1997 and 2007 in kids under 18 -- and no one knows why the condition is on the rise.
A 2010 study in the journal Pediatrics found that 8% of children younger than 18 in the United States have at least one food allergy. Among those with food allergies, about 39% had a history of severe reaction, and 30% were allergic to multiple foods.
Peanut allergy is the most common food allergy, according to the study, followed by milk and shellfish. In fact, according to the Centers for Disease Control and Prevention, more than 90% of allergic reactions come from just eight foods: milk, eggs, peanuts, tree nuts, fish, shellfish, soy and wheat.
"Most of the fatalities that I'm familiar with have been associated with peanut," Bassett said.
Allergic reactions can appear to subside but reemerge much later, a phenomenon called "biphasic reactions." A second wave of an allergic reaction can occur up to 72 hours after the first one, Bassett said, but in most cases it's sufficient to monitor a patient for eight hours after a severe anaphylaxis episode.
People with extremely sensitive allergies cannot risk eating anything that may have come into contact with the foods they can't eat, Bassett said, which is why people should read food packaging labels extremely carefully and take seriously warnings like "May contain traces of peanuts."
Anyone with a history or risk of food allergy should get evaluated by a certified allergist and come up with an action plan for prevention and treatment, Bassett said.
Parents should communicate with camps, schools, relatives, restaurants and anyone who might be serving food to their allergic child about what foods to avoid and how serious the condition needs to be taken.
"It's essential when you have a serious, life-threatening problem like this to have a plan in place ahead of time," Bassett said. "With the best intentions, we generally get good outcomes, but this is an example of something that is obviously a horrible tragedy."
Natalie was aware of her food allergy and "took every care," the Rev. Michael Kiernan of Our Lady of the Assumption Church in Carmichael, California, told KXTV.
Natalie's symptoms didn't begin immediately when she spit out the treat at Camp Sacramento, according to the local station.
When she reached for the snack at camp, she didn't know that it was made with peanut butter. For about 20 minutes, she felt fine, but then she started vomiting, had difficulty breathing and went into cardiac arrest.
An ambulance took her to a hospital, where she was pronounced dead.
Her family told KXTV that Natalie had aspirations of becoming a neonatologist so that she could care for premature babies, such as herself and her twin sister.
"While our hearts are breaking over the tragic loss of our beautiful daughter Natalie, it is our hope that others can learn from this and realize that nut and food allergies are life threatening," Natalie's family said in a written statement to KXTV. "Caution and care for those inflicted should always be supported and taken."