Story highlights
In a rare event, organ donor Paul Hawks, 56, died during transplant surgery
Hawks' pre-operative EKG was abnormal, but he had surgery anyway
Lifesaving blood pump nearby wasn't used to help Hawks
Health officials say they have no "position on what caused the patient's death"
Before dawn on her 57th birthday, Lorraine Hawks and her husband, Paul, piled into their brother-in-law Tim Wilson’s Lexus in Pelham, New Hampshire, with Lorraine and her sister Susie in the back seat and the men up front. As the two couples drove to the Lahey Clinic in Burlington, Massachusetts, Lorraine and Paul teased Tim mercilessly.
“By 5 o’clock today, you’re going to have a Republican liver!” they taunted Tim. “You’re going to love Ann Coulter! You’re going to love Glenn Beck!”
“No way!” protested Tim, a staunch Democrat. He swore that even with a chunk of his Republican brother-in-law’s liver inside him, he’d never be conservative. The foursome joked and laughed during the 45-minute drive to Lahey. At the hospital, the sisters kissed their husbands goodbye, and the men were wheeled into operating rooms, where surgeons would remove 60% of Paul’s liver and give it to Tim, who suffered from advanced liver disease.
As Lorraine sat in the waiting room with Susie that May morning two years ago, she prayed her husband’s liver lobe would cure her brother-in-law. She prayed for her husband, too, but she was less worried about him, since she says the surgeons had reassured them while liver donation wasn’t without risks, it was safe for Paul, a 56-year-old man in good health.
Neither of Lorraine’s prayers came true. Tim died less than a year later, after receiving the transplanted part of Paul’s liver. He was 58. Her husband died that very day on the operating room table.
“We walked into the hospital a married couple, and I left the hospital at the end of the day as they loaded my husband onto the coroner’s truck,” says Lorraine, who has hired a lawyer and plans to file a lawsuit against the hospital.
‘He didn’t hesitate to say yes’
Paul Hawks, an electrician for the Florida Department of Transportation, was one of more than 4,500 people in the United States in the past 25 years who have donated a section of their liver while still alive. Death is rare: Besides Paul, three other donors have died since 1999.
The relatives of the other donors – they died in 1999, 2002 and 2010 – have gone public, but this is the first time Lorraine has discussed her husband’s death.
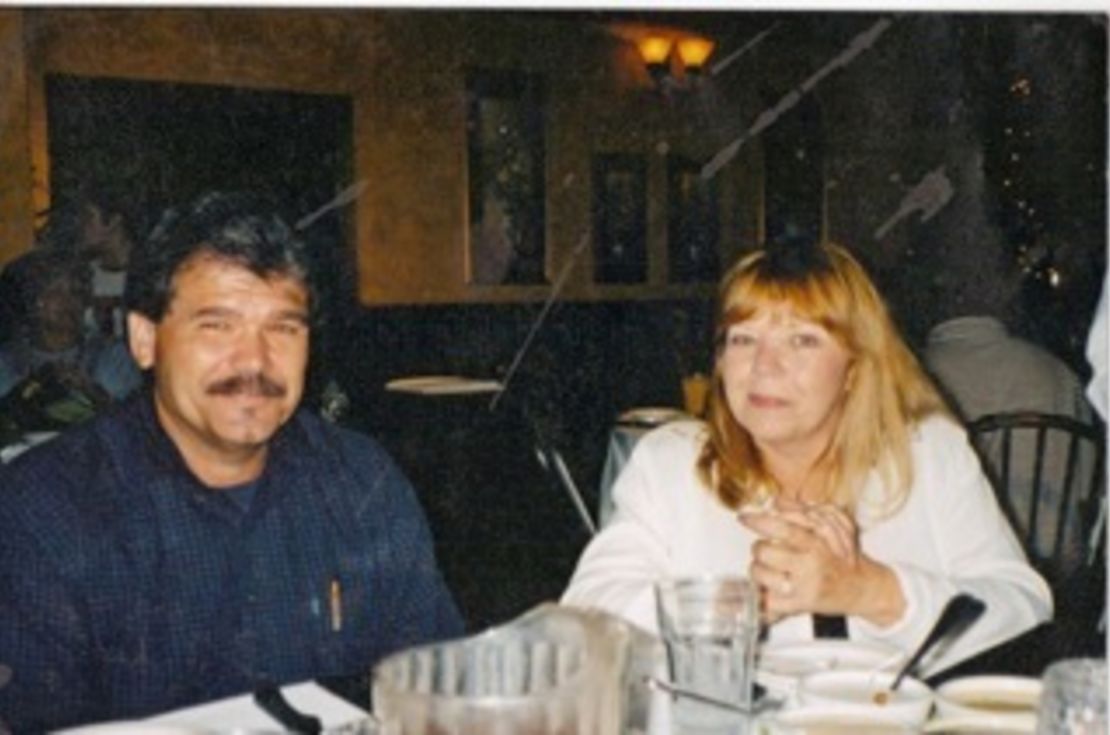
“I want everyone to know what a generous, wonderful man Paul was. When he found out Tim needed a liver, he didn’t hesitate to say yes,” said Lorraine, a school bus aide for children with special needs in Tampa, Florida. “They weren’t blood relatives, but they were a perfect match, and he felt privileged that God was going to let him help Tim regain his health.”
Living organ transplants are a miracle of modern medicine. In all, more than 100,000 people in the U.S. like Paul have donated a kidney, a liver lobe or another body part while still alive to save someone else’s life. Most of the time, the surgeries go well. Not only are donor deaths rare, but major complications of any kind are the exception rather than the rule.
This makes it all the more difficult for Lorraine to understand why her husband was one of the few who didn’t make it.
‘We tried very hard to save Paul …’
After her husband was wheeled into surgery, Lorraine, her father-in-law and Susie walked around the block a bit and got a bite to eat in the hospital cafeteria. Then shortly after 1 p.m., about four and a half hours after the surgery began, Lorraine says, the coordinator of the transplant team came out to talk to them.
Sitting next to Lorraine, their knees nearly touching and speaking in a near whisper, Lorraine says, the coordinator told her that they were having trouble getting Paul’s blood to coagulate and that an expert had been called in. Then about an hour later, the coordinator came out again to say her husband was having “irregular heart rhythms.”
“She was acting real strangely, and we were so frightened,” Lorraine remembers.

The coordinator’s cell phone rang, and she answered it. She hung up and rubbed Lorraine’s arm, which Lorraine found strange, and told her she’d be back in five minutes.
When she returned, she asked the family to come into a small private waiting room. Lorraine remembers her father-in-law screaming, “Tell me what happened to my son!” But the coordinator wouldn’t say anything. The family sat there for about 40 minutes. Then the coordinator asked the family to go into a conference room farther away from the waiting area.
“We’re looking at each other and said ‘this can’t be good,’ ” Lorraine recalls. “We walked, crying, holding onto each other.”
Suddenly the conference room filled with doctors, counselors and pastoral staff.
“We tried very hard to save Paul …” Lorraine remembers one of the doctors saying. She was sobbing so hard she didn’t hear the rest of his sentence. Then the surgeon who did Paul’s operation, her eyes red and puffy, got down on her knees to speak with Lorraine eye-to-eye.
“I saw her mouth moving, but I couldn’t hear what she was saying,” Lorraine remembers. “My brain was on fire.”
Lorraine stayed with her husband’s body until the coroner came to take him away. She says the next day, people from the hospital called her six times, offering condolences and to pay for Paul’s funeral. She didn’t want to talk to them.
A few weeks later, back home in Tampa, Lorraine read a statement online from the Lahey Clinic’s then-CEO, Dr. David Barrett.
“Lahey Clinic and its transplant team are extremely saddened by the loss of a gentleman who died while donating a portion of his liver to his relative,” Barrett said. “Since the inception of its live donor liver transplantation program in 1999, Lahey Clinic has performed more than 200 of these complex life saving surgical procedures.”

Reading the article made Lorraine feel worse, she says. It still didn’t explain why her husband had died.
Then in July, about two months after her husband’s death, Lorraine stopped by her post office after grocery shopping to pick up her mail. In her box was a thick envelope from the Massachusetts Department of Public Health. Inside was a nine-page report with the details of what happened during Paul’s surgery.
Finally, she thought, her questions would be answered. Finally, she would find out why her husband died.
‘Donor … could not be resuscitated’

The Department of Public Health report gives a rare and gruesome picture of a surgical procedure gone horribly wrong.
The department’s account is based on medical records, operating room communications and two days of interviews with the attending transplant surgeon and other doctors, nurses and administrators.
After Lorraine and Susie kissed their husbands goodbye, Paul and Tim were wheeled into separate operating rooms. Everything went fine until about four hours into the operation, when a vein that carries blood away from the liver partially tore off and started bleeding.
Paul’s surgeons immediately called for assistance. More doctors and nurses arrived in his operating room. It was to be the beginning of a 2½-hour fight to save Paul.
The partially torn vein came all the way off, and doctors sewed up that tear, but then they noticed bleeding coming from somewhere else. As they searched for the source, a clamp on a vein got knocked off, injuring the vein. Repairing that injury, they noticed more tears. They fixed those tears, all the while giving Paul blood products and drugs to raise his blood pressure.
It seemed like Paul might be getting better, but then he started to bleed from several areas all at once. His heart started to beat very fast. Doctors performed CPR, and when that failed, they cut his chest open, massaged his heart directly and shot drugs into his heart to get it going again. But none of it worked.
“The patient had a cardiac arrest secondary to excessive bleeding & could not be resuscitated,” the report states.
Paul Hawks was pronounced dead at 3:01 p.m. on May 24, 2010.
Pamela Johnston, a spokeswoman for the Lahey Clinic, one of the largest liver transplant centers in the country, declined to comment about the details in the state’s report. Lahey voluntarily stopped operating on living liver donors for about four months.
The Massachusetts Department of Public Health did not cite the hospital for any deficiencies. The Lahey Clinic conducted its own internal investigation into Paul’s death and hired outsiders to conduct an external investigation. Lahey declined CNN’s request for copies of both these reports.
More red flags
Lorraine read the Department of Public Health report sitting in her car in the parking lot of the Tampa post office. As she read the details of her husband’s failed surgery, she wondered whether all the tears and bleeding were anyone’s fault, or were they just unavoidable consequences of surgery, inevitable events that statistically speaking happen sometimes, and Paul was just unlucky?
Three other items in the Department of Public Health report raised even more questions.
First, she found out Paul had been given a pre-operative EKG, and it was abnormal. It showed he might have had a past heart attack, but then follow-up testing showed no evidence of poor blood flow to his heart.
“I had no idea he’d had an abnormal EKG,” she says now. “If I had known, I never would have let him have the surgery.”
The report doesn’t say whether Paul knew about his abnormal EKG or if a cardiologist was called in to evaluate whether his heart was strong enough to tolerate surgery. Johnston, the Lahey Clinic spokeswoman, declined to answer questions about the EKG or about any aspect of Paul’s surgery or pre-operative care.

Second, the report pointed out that a special high-speed blood pump wasn’t used to give Paul blood.
The $20,000 device pumps blood at least three times faster than other pumps. Called a Belmont Pump, it’s saved soldiers’ lives as they lay massively bleeding on battlefields in Afghanistan and Iraq.
Lahey owns a Belmont Pump. At the time of Paul’s surgery, it was nearby in Tim Wilson’s operating room. But as Paul lay bleeding to death for 2½ hours, no one brought it in to his operating room.
“It’s portable,” says George Herzlinger, president of Belmont Instrument, which makes the device. “It weighs 27 pounds. You just wheel it over.”
Third, the report describes how Paul’s surgeons never activated a set of procedures used when a patient is massively bleeding.
Called the “Massive Blood Transfusion Protocol,” it directs surgeons to call the hospital’s transfusion services and activate a set of procedures so a patient who’s bleeding profusely can most efficiently get the blood products he needs.
The report notes that surgeons thought none of these things – the abnormal EKG, the lack of the high-speed pump, the inactivated protocol – contributed to his death.
Nonetheless, the report shows the hospital did think it could have done some things differently.
After Paul’s death, staff members questioned whether there needed to be a “higher standard” when evaluating patients with abnormal EKGs. They said it would have been “nice” to have had a Belmont Pump in the room. They educated staff about activating the blood transfusion protocol.
A new type of surgery
In the end, the Department of Public Health report didn’t answer Lorraine’s questions as she’d hoped. She still didn’t know what had killed her husband. Nearly two years after her husband’s death, she still has no peace and no closure.
“DPH does not have a position on what caused the patient’s death,” Jennifer Manley, a DPH spokeswoman, explained in an e-mail to CNN. “Likewise, we don’t look at who is to blame for the death.”
Lorraine was emotionally spent. While she had the support of her sisters and her sons, she wanted something more.
“I wanted to talk to a widow, to someone else who’d gone through this,” she said.
So Lorraine typed “donors that died” into Google. It didn’t take her long to find Vickie Hurewitz, whose husband, Mike, was the donor who died in 2002. She found Hurewitz’s e-mail address, and they set up a time to talk on the phone.
“I cried with her for two hours. Sometimes I couldn’t even talk, I was crying so hard,” Lorraine remembers. “Vickie said to me, ‘Lorraine, I’m so sorry. I know your heart is broken.’ “
At the end of the conversation, Vickie said, “Lorraine, I want you to meet a friend of mine.”
That friend was Donna Luebke. A nurse in Ohio, Luebke donated a kidney to her sister in 1994. Now an associate at the Center for Biomedical Ethics at Metrohealth Medical Center and Case Western Reserve University in Cleveland, Luebke has developed an interest in the ethics of living organ donation.

Working with Luebke, Lorraine found out there was something else she didn’t know about Paul’s surgery.
Most liver donors in the United States have “open” surgeries with a long incision across the abdomen. According to medical records obtained by CNN, Paul had laparoscopically assisted surgery, a minimally invasive technique with three very small cuts.
The advantage of “lap-assisted” surgery is a much easier recovery for the patient. The downside, surgeons say, is if a patient starts bleeding, it can be harder to find the source, since they can look only through small incisions rather than a very large one.
“It’s harder to see, especially if you’re not used to doing this surgery,” Luebke says.
Luebke told Lorraine she thought the Lahey surgeons might not have had much experience with “lap-assisted” surgeries on liver donors. The technique had only been used for a few years in the United States when Paul had his surgery, and some surgeons were trying it out for the first time.
“There’s a steep learning curve,” she says. “It’s a different skill set than doing an open surgery.”
Dr. Peter Pronovost, a patient safety expert at Johns Hopkins University School of Medicine in Baltimore, agrees.
“When a surgeon wants to try out a new surgical technique, they can just go ahead and do it,” he says. “There’s no rule saying you have to tell the patient you’re taking out the liver in a different way and this will change the risk profile.”
A spokeswoman for Lahey declined to say how many laparoscopic liver donor surgeries had been done at Lahey before Paul’s operation.
A widow’s regrets
Three months after Paul died, Ryan Arnold died after donating a liver lobe to his brother in Colorado. His death received a great deal of media attention, and the American Society of Transplant Surgeons released a statement.
“Living donor procedures are not without risk to the donor, even in experienced hands and programs,” the statement read. “While attempts are always made to minimize donor risk, complications including death are always possible.”
Now, nearly two years after her husband’s death, after poring over the Department of Public Health report and her husband’s medical records, Lorraine still wonders whether she could have done anything to keep from losing her husband on her 57th birthday.
She says there’s one thing she knows she would have done differently. She had only enough time off work to fly from Florida to Boston for the surgery itself, so she wasn’t there for Paul’s pre-operative testing. He did that on his own.
Source: United Network for Organ Sharing (UNOS)
“God, how I regret that,” she says. “I would have asked a million questions.”
Now she wonders whether Lahey gave Paul all the information he needed to make a smart decision about whether to go under the knife.
An inspection seven months after her husband’s death by the federal Centers for Medicare & Medicaid Services (CMS) revealed that Lahey violated several federal rules for informing and protecting donors.
Under these regulations, each donor is supposed to be told about how other organ donors fared after their surgeries, both nationwide and at Lahey specifically. Studying the records for seven liver donors, CMS found Lahey failed to provide all of them with the most current surgical outcomes.
Dr. Roger Jenkins, the chairman of surgery at Lahey when Paul died, agrees that the data wasn’t as up-to-date as it should have been.
“It got caught in the paper shuffle that’s part of the hospital’s record keeping,” he said.
The CMS report noted that Lahey was out of compliance in another area.
Transplant centers are supposed to assign a staff person, such as a doctor or social worker, to be an independent advocate for the donor. The donor advocate is supposed to take into account only the donor’s concerns – for example, in Paul’s case, the abnormal EKG findings – and not the concerns of the recipient, since sometimes there can be a conflict of interest between the two.
To make sure the advocate is focused solely on the donor, there’s supposed to be a “wall” between the donor advocate and the recipient’s team, but federal inspectors observed Lahey’s donor advocate going on medical rounds and participating in meetings run by the recipient’s team.
“This goes against (federal) policy,” the inspectors wrote in their report. “Their roles were not clearly defined to ensure protection of the rights of living donors.”
Jenkins says he didn’t know that the donor advocate wasn’t supposed to attend meetings about the recipient.
“We interpreted the rules one way and the CMS reviewer interpreted them another way,” Jenkins says. “There was certainly no intent not to comply with CMS regulations.”
He added that it’s not uncommon for hospitals to be out of compliance with CMS rules.
“If every center doesn’t have at least one or two major out-of-compliance issues, that would be surprising to me,” says Jenkins.
According to CMS, the hospital corrected the problems and was back in compliance with federal regulations about three months later.
‘A very, very strong faith’
Lorraine knows she may never get all her questions answered about why her husband died that May afternoon.
She looks back on the day Paul made the decision to donate part of his liver with a mixture of sadness and pride. It was Thanksgiving Day, 2009, and they were at a Cracker Barrel in Tampa with their two grown sons.
During dinner, Lorraine’s cell phone rang. When she answered the call and heard Susie crying, Lorraine excused herself to take the call outside.
When she returned to the table, Lorraine told Paul and their sons the bad news.
“Tim is ill, and if he doesn’t get a liver donation, he’ll die,” she told them. Getting a liver from a cadaver was out of the question, she explained, since Tim was so sick, he’d never live long enough to get off the waiting list.
“My husband in 30 seconds – no, less than that – said ‘I’ll get tested,’ ” Lorraine remembers.” And then our son Joseph said he’d get tested, too. Nobody ever asked them to do it. They just did it.”
Before Joseph could protest, Paul told his son he’d fly to Boston first to get tested first, and if he wasn’t a match, then Joseph could try. That turned out not to be necessary, as the tests showed Paul was a “perfect match,” Lorraine says.
Before Paul flew to Boston for the transplant, the couple’s other son, Gene, saw his father off at the Tampa airport.
“We had lunch together, and then right there in the middle of the airport I hugged him, even though he wasn’t a touchy-feely guy,” Gene remembers. “I prayed for good surgeons’ hands to do the right thing.”
In retrospect, Gene wishes he had advised his father to get a second opinion from another doctor about whether he was healthy enough to give away 60% of his liver – from a doctor who didn’t stand to financially gain from the transplant.
But his family says before the transplant, Paul Hawks wasn’t looking for advice. He was looking to do good. Being a living donor was just an extension of the goodwill he did in his regular life, they say, like helping elderly people in his church with their home repairs for free.
“He wanted people to see Christ in him every day with every interaction,” Gene says. “At lunch that day, he told me he wasn’t going to die, because it was low risk, but if he did, he was prepared for it, because he was going to heaven.”
CNN’s Matt Sloane, Jennifer Bixler and John Bonifield contributed to this report.



