Editor’s Note: Psychologist John Duffy, author of “Parenting the New Teen in the Age of Anxiety,” practices in Chicago. He specializes in work with teens, parents, couples and families.
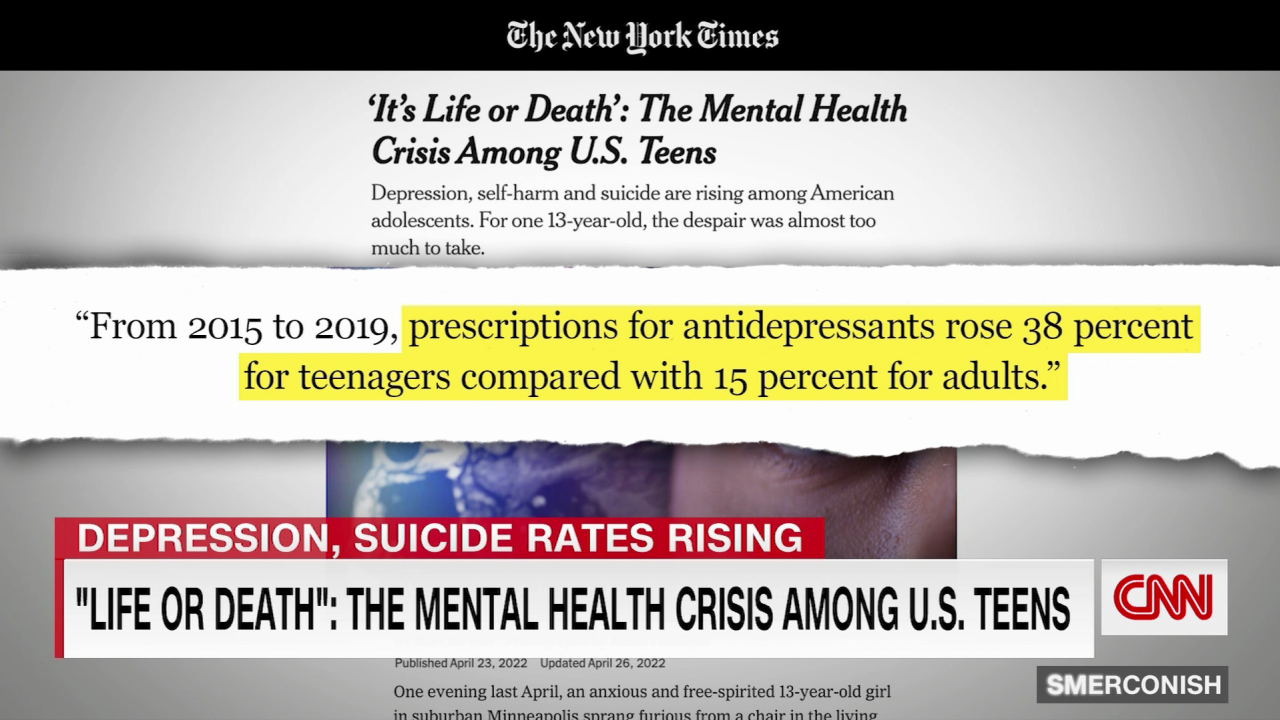
There’s a crisis in teen mental health, suggesting a marked increase in mental illness, sadness and teen hopelessness, according to the US Centers for Disease Control and Prevention. These findings leave many experts wondering whether the pandemic drove an increase in diagnosable mental health disorders in teenagers or if the impact of Covid-19 exacerbated the symptoms of teens already struggling emotionally.

As a psychologist with experience treating tweens and teens, I’ve seen more children in my office saying their anxiety, depression and attention issues were getting significantly worse. I wondered if my experience was typical, so I turned to Dr. John Walkup, chief of child and adolescent psychiatry at Northwestern University Feinberg School of Medicine and head of the Pritzker Department of Psychiatry and Behavioral Health at the Ann & Robert H. Lurie Children’s Hospital of Chicago.
Walkup said he believes that the pandemic has not driven an increase in the incidence of mental illness among teens – but it has “unmasked symptoms” that may have otherwise been managed.
I spoke with Walkup to discuss his research findings and address what parents and caregivers can do to help their children right now.
CNN: You say that we are not seeing much new mental illness in children over the past two years? What we’re seeing are difficulties that have been exacerbated by the pandemic, correct?
Dr. John Walkup: Yes. You know, 20% of kids have a mental health problem before they graduate from high school on average across the United States. Only half of those kids get some kind of assessment or treatment, and of that population only about 40% of them get clinically meaningful benefits. That’s about 15% of kids who have a mental health issue getting help. Then take away school, family, peer support and sports, and you force them to stay home. You know those kids are not going to do well over time.
There is probably a small group of kids who get long Covid where you might say that there is some direct impact of the Covid virus on the brain, but that’s a pretty small group of kids. But overall, when we think about what Covid has done, it has really destroyed the infrastructure for kids with mental health problems. If you really think about it in a slightly deeper way, we’ve been advocating for mental health for kids for a long time. Families and schools are more aware of mental health issues, so you’ve now got this kind of perfect storm of increased awareness and increased advocacy, resulting in an increased need for care. And the structure for that care has fallen away over the past two years.
CNN: Given those numbers, do you feel that the pandemic will shine some light on the mental health needs of kids that we wouldn’t have seen without this crisis?
Walkup: I think we would have seen an increased awakening either way because the advocacy efforts are there. We now have effective treatments for every major psychiatric disorder for kids, and the treatments are good. Once you have treatments, you can advocate effectively, right? So before the pandemic more and more kids were therefore coming for care, good care. But then when you strip away all of the support infrastructure (school, activities, etc.), those kids are going to become symptomatic much more quickly. Without that infrastructure, we’ve seen a dramatic, unexpected rise in pathology.
CNN: You’ve highlighted a distinction between mental illness and distress. What’s the difference?
Walkup: Anxiety and sadness are normal human emotions. Anxiety helps us prepare for difficult outcomes, and sadness helps us get closer to people. What we work on in terms of mental illness are pathological forms of anxiety or sadness. That’s clinical depression and the anxiety disorders, and those things are qualitatively different than normal human sadness or normal expectable and proportional anxiety.
During Covid-19, when kids didn’t know what to expect, they would have increased rates of normal anxiety and distress because they’re not with their friends and they’re not at school. They have questions about their future. But that’s not pathological. That’s expectable, proportional and understandable, and it will go away when things normalize.
CNN: You also suggest the pandemic has exerted a higher impact on girls and the LGBT community. Any idea why that might be?
Walkup: When the pandemic hit, more kids who were untreated or poorly treated began to present for care. The prevalence of anxiety and depression for young females is greater than that for males, which may account for disproportionate treatment seeking. More girls have needed help that hasn’t been there in the last two years.
In the LGBT community, those youngsters struggle. It’s hard to be different when you’re a young person. This group also experiences higher rates of bullying. Many feel they do not necessarily fit in even within their own families. So you would expect that those kids would really struggle during this period of time, and they have.
CNN: What risk factors should parents and caregivers be looking for now?
Walkup: This is really important. Parents should look at their family history. If there’s a psychiatric disorder rattling around somewhere in that family history, be aware that these things are genetic. They pass from one generation to the next. It’s also important for parents to understand that these psychiatric disorders arise at very predictable times in development. Kids with ADHD present between ages 4 and 7. Kids with anxiety disorders present between ages 6 and 12, and kids first present with depressive disorders in the mid-teenage years.
So, if you have a family history of ADHD, you should be looking for ADHD symptoms in your 3-, 4- and 5-year-olds. If you have an anxiety disorder in your family history, you should be looking for anxiety between 6 and 12 years old and similarly with depression. Share that information with your pediatrician. Your pediatrician knows what these symptom presentations look like so you can get on top of it really early.
CNN: You’re saying don’t wait for a symptom profile to present itself in your child? Be proactive.
Walkup: Right. If you have an ADHD family history and you’ve got a 2- or 3-year-old child, get really good at parenting because these kids are tough to parent. If you have a family history of an anxiety disorder, Mom and Dad should make sure that they’re both in good emotional shape. You’ll need to become fearless because we know that the treatment for anxiety is taking on those things that are scary or challenging. We also know for families where there’s a strong depression history that getting physically active and being engaged in the world is the best behavioral treatment.
If you know your family history, you know the age of onset risk, you know what the things are that you can do to mitigate that risk once the condition arises. Your child is going to be in much better shape and easier to treat if all of that work was done before the symptoms actually manifest.
CNN: What can parents or caregivers do now to help their children mitigate any emotional difficulties resulting from the Covid-19 pandemic?
Walkup: Take a deep look at your family history and don’t just attribute all symptoms to Covid. If you have a strong family history and you see symptoms in your kid, don’t discount it. Take it seriously. Learn and read and talk to your pediatrician because they know about these conditions. They will start laying the groundwork for intervention. If you don’t need intervention now, laying the groundwork and getting prepared is much better than being surprised by a condition later.
Families often hire a financial adviser or a legal adviser. Why not have a mental health adviser if you have a family history of a psychiatric disorder? Get that mental health adviser working with you early around prevention and early intervention. If you begin to take care of these conditions early, you can minimize the impact. If you don’t, you risk maximum impact on long-term outcomes.
CNN: Do you feel hopeful going forward about the mental and emotional well-being of our kids?
Walkup: I think we have great treatments, and if we can get kids to treatment, we’re going to be OK. We do have a lot of “anti-treatment” sentiment in this country and a lot of discounting of the mental health pandemic. We don’t take it seriously enough, so my feelings are mixed. If we get kids into care, we do very well with them. They respond well and get better. On the other hand, there are so many hurdles that families have to jump over to get care nowadays. This can make it difficult for kids to get the care they need.
Overall, we will see a huge decrease in the mental health burden on kids simply because parents and guardians will figure out how to get ahead of emotional difficulties. That parental leadership within a family can mitigate a lot of heartbreak.