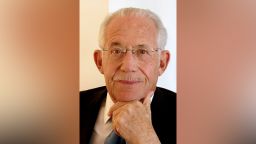
Editor’s Note: William Haseltine, PhD, is chair and president of the global health think tank, ACCESS Health International. He is author of numerous books, including the recently released, “A Family Guide to COVID-19: Questions and Answers for Parents, Grandparents and Children.” The views expressed in this commentary are his own. View more opinion on CNN.
A lot of hope has been placed on the possibility of a Covid-19 vaccine by the end of this year.
However, overcoming the technical challenges of developing a vaccine – and the safety issues inherent in making one that works for the populations most at risk – is no easy feat.
While it may be possible to deliver a vaccine by the end of this year, absolutely every step of its development would have to go perfectly. From experience, I can tell you how rare that is.
Vaccines don’t act as impenetrable shields that prevent viruses from entering our bodies. Rather, they teach our bodies how to rapidly mobilize our immune defenses against a foreign invader. The rapid immune response helps us clear the virus from the body before it wreaks its damage.
But in the case of Covid-19, according to one study, not everybody infected by the virus makes the neutralizing antibodies that are necessary to clear the virus and fewer still make them in high numbers. What we know from nearly 60 years of observing coronaviruses is that even if a body’s immune system can clear the virus, the pathogen can likely reenter the system and cause illness again.
Of the more than 100 vaccines currently in development, the ones tested on primates have not prevented nasal infections, though in one case the vaccine prevented the disease from spreading to the lungs where it is known to cause severe damage. However, since Covid-19 progresses somewhat differently in monkeys than in humans, it’s hard to know how effective these vaccines will be in human trials.
One thing we do know is that some of the vaccines currently being tested in humans are already causing serious side effects. The side effects are likely a result of the powerful ingredients added to the vaccine to help inflame the body’s immune system. These ingredients – called adjuvants – help vaccines work better, but if they can land the young and healthy patients in the clinical trial in the hospital because of high fevers and fainting, imagine what they might do to those already ill with secondary conditions or to those who are older. Indeed, the elderly may need repeated doses of the vaccine, given how resistance to some vaccinations becomes progressively more profound with time.
But even without a vaccine, there is reason for hope that a medical solution to the crisis will soon be at hand. It will likely take the form of anti-Covid drugs that will be able to treat patients newly infected and prevent others from becoming ill. These drugs can likely help us bridge the gap between where we are today – with only masks, hand hygiene and physical distancing to protect us – to where we hope to be tomorrow – with a vaccine in hand.
Recent studies have shown two types of drugs with particular promise. The first are antivirals – drugs that act on the virus itself and prevent it from replicating. Antivirals generally target either the enzymes a virus needs to copy its genome (polymerases) or those needed to cut larger proteins into smaller functional fragments (proteases). Coronaviruses, in general, are a target-rich environment for antivirals and this coronavirus, SARS-CoV-2, is no different than the others since it uses an active protease, a key protein responsible for the reproduction of the virus, to copy itself.
In a study published last month in Science, researchers announced their discovery of two new drug candidates that inhibit the SARS-CoV-2 protease. In test tube experiments, they found that the chemicals could bind to the protease and prevent replication, with one of them – a chemical designated 11a – more promising than the other. Chemical 11a will soon be tested for safety in humans, but early results from this study in dogs and mice suggest that the drug is both effective and non-toxic.
The other set of drugs showing promise are monoclonal antibodies, which are lab-created antibodies that work by blocking SARS-CoV-2 spike proteins from attaching to the ACE2 cell receptors in our body. By blocking the attachment, they prevent infection altogether. In another study published in June in Science, a separate set of scientists discovered two antibodies that each prevented different parts of the SARS2 spike protein from binding to the ACE2 receptor. While each of the antibodies on its own can neutralize the virus, together they are even more effective at preventing infection.
Just this week, late stage trials were announced for another double antibody cocktail that will be tested in 2,000 people across the United States for their ability to prevent infection and treat those in the early stages of Covid-19. With this drug – and with the other set of monoclonal antibodies already researched – there is a question of whether they are going to be effective against a virus like SARS-CoV-2 that lives primarily in the nose and the lungs instead of in the blood. That said, monoclonal antibodies have worked against the respiratory syncytial virus, which has many similarities to SARS-CoV-2.
Much like the vaccines that have showed early promise, these drugs too will need more testing before their safety and efficacy can be proven. But the timeline for testing these drugs is much shorter than for a vaccine, in large part due to how quickly and easily their efficacy can be determined. For antivirals and monoclonal antibodies, you know whether the virus works within a matter of days – either the viral load in the patient goes up or it goes down – and with very few individuals. Our first effective treatment for HIV, an antiviral, was proven in a group of just 19 patients given the drug.
What this means is that even if our path to a Covid vaccine is much longer and harder than we currently estimate, we can still have drugs in hand as early as the beginning of next year that can keep those most vulnerable from becoming infected and could, potentially, treat those already ill.
The science will eventually save us. In the meantime, we must use what we know for certain will work today – masks, physical distancing and quarantine – to reduce lives lost unnecessarily while we wait.





