Editor’s Note: Dr. Tom Frieden is the former director of the US Centers for Disease Control and Prevention, and former commissioner of the New York City Health Department. He is currently president and CEO of Resolve to Save Lives, a global non-profit initiative funded by Bloomberg Philanthropies, the Chan Zuckerberg Initiative, and the Bill and Melinda Gates Foundation, and part of the global non-profit Vital Strategies. Resolve to Save Lives works with countries to prevent 100 million deaths and to make the world safer from epidemics. Dr. Frieden is also senior fellow for Global Health at the Council on Foreign Relations. The views expressed in this commentary are solely those of the author.
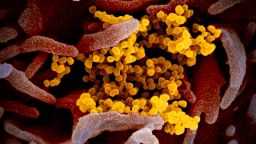
Last week, I noted that we were in the calm before the storm. Now, the storm has started in the United States and is gathering strength. Covid-19, the illness caused by the novel coronavirus, has passed 100,000 cases globally.
There are already clusters of infection in several areas of the country. Financial markets are in turmoil, global travel is grinding to a halt, and many people worry about the safety of travel, work, school and meetings.
Covid-19 will get a lot worse before it gets better.
Nursing homes are ground zero for Covid-19
One thing stands out as the virus spreads throughout the United States: Nursing homes and other long-term care facilities are ground zero. Most deaths in the United States thus far are connected to a single nursing home in Kirkland, Washington.
This is not unexpected. There have been influenza and other disease outbreaks in nursing homes in the past. Influenza causes severe nursing home outbreaks even though we have influenza vaccines and medications – tools we lack for Covid-19. Residents in nursing homes are older and sicker and live in close quarters. Staff at these facilities are also at high risk. They are in close contact with many residents every day, and infection control is often suboptimal.
This nursing home outbreak of Covid-19 is what we call a “sentinel event”: a warning of outbreaks and deaths that may be coming. But these deaths are not inevitable. It is essential that we protect the most vulnerable people – those with serious underlying health conditions such as respiratory disease, cancer and diabetes and older adults. The overall case fatality ratio for Covid-19 appears to be under 1%, but is many times higher for the elderly.
The threat of rapid spread within long-term care facilities means that if we make the tough decision, now, to immediately restrict visits, we may be able to prevent many more outbreaks like the one in Kirkland. We also must ensure that any nursing home staff who are ill not come to work – and that they receive paid leave, so they have no economic incentive to come to work if ill. Families want to visit loved ones; we should facilitate virtual visits until we know more and can do more to protect the most vulnerable.
What else can we do right now to keep Covid-19 from getting even worse?
There are other actions we can all take now to minimize further spread of Covid-19 and prevent even more societal and economic disruption.
Everybody. We must all make preventing spread of infection a top priority. That means frequent and thorough hand washing (or use of hand sanitizer), covering our coughs and staying home if we’re sick. Seek medical attention if you have Covid-19 symptoms (dry cough, fever, difficulty breathing) for more than two days. And don’t wear a face mask unless you have cough or fever. Outside of health care settings, a mask’s main benefit is to help keep someone who is sick from infecting others. We aren’t going to have enough masks, and we need to prioritize those that we have for health care workers, those caring for ill people and people who have symptoms.
People who are medically vulnerable. Medical vulnerability is not about chronological age but about how healthy people are. A healthy and vigorous 79-year-old is almost certainly at lower risk than a 55-year-old with diabetes and lung disease. People who are medically vulnerable will stay safer if they avoid large-group meetings, crowded enclosed spaces (including airplanes) and they may want to telework and stay 6 feet away from others as much as possible, as well as limit the number of people they come into contact with.
Health care providers. Hospitals and other health care facilities need to prepare to surge safely. Strict infection control procedures must be implemented in all areas of every facility, including proper triage of every patient and isolation of all suspected cases. As in a busy flu year, hospitals should be ready for a surge of people with mild symptoms and the “worried well” – people concerned that every cough might mean they have Covid-19. If there is lots of severe illness, it may become necessary to postpone elective surgery, train nurses to provide respiratory therapy and expand the number of patients who can be supported with intensive care.
Society and government. We need to hear from the world’s leading experts, including Drs. Anne Schuchat and Nancy Messonnier at the US Centers for Disease Control and Prevention, and Dr. Anthony Fauci at the National Institutes of Health. We need them to speak to us every day to keep Americans informed about what we are learning, the spread of the virus and what people can do to protect themselves. Clear, credible and consistent information about the virus and the response is urgently needed. Political leaders must take a hard look at the costs and benefits of social distancing interventions. Canceling large public gatherings, switching to telework, and considering closing schools is disruptive, but may be needed in the short term to prevent more severe longer-term impact. At a minimum, we must reduce the risk to medically vulnerably people now.
Get CNN Health's weekly newsletter
Sign up here to get The Results Are In with Dr. Sanjay Gupta every Tuesday from the CNN Health team.
Our understanding of Covid-19 is changing daily – even hourly – and we need answers to important questions so we can respond as effectively as possible. For example, it’s now clear that children do get infected but rarely get sick. We don’t know whether they are a major source of the spread of infection to others, and therefore whether closing schools would decrease spread as it does with influenza. We will learn more and adjust our protective actions as we do, but we know enough to take decisive steps now. What we do now and in the coming few weeks will help determine how extensively and rapidly this novel coronavirus spreads and how much death and disruption we prevent.