Story highlights
- Scientists worldwide are seeking improved and universal flu vaccines
- In one new study, researchers turn to a mutant virus to design a vaccine
(CNN)As a deadly flu season continues to ravage the United States, scientists are scrambling to find new ways to fight the virus, including building vaccines that offer stronger protection against the most aggressive flu strains and last longer than just one season.
One new study offers a novel approach to developing such a vaccine.
Scientists have used a mutant influenza A virus to develop a vaccine that gave the immune systems of mice and ferrets a significant boost, according to the study published in the journal Science on Thursday. The newly designed vaccine has been tested only in those lab animals, and more research is needed to determine whether it could be used safely and effectively in humans.
Yet the researchers hope that, once more studies are conducted, this vaccine could "reduce the spreading of influenza viruses in the world," said Ren Sun, a professor of molecular and medical pharmacology at the David Geffen School of Medicine at University of California, Los Angeles, and the study's senior author.
"We expect it to be effective in humans, but there are possibilities for potentially unexpected outcomes," Sun said, adding that, if proven to be effective, the potential vaccine could possibly be administered as a nasal spray.
"It will be easier for more people to take flu vaccine," he said, if used as a nasal spray at home rather than an injection by a health care professional, for instance. Though, he added, it could take "several years" before such a potential vaccine would even begin the FDA approval process. (There's one approved nasal seasonal flu vaccine, FluMist, however it is not currently recommended by the US Centers for Disease Control and Prevention because it's less effective than an injected vaccine.)
The new study sheds light on one innovative and emerging approach to building a robust flu vaccine, at a time when the US is experiencing widespread and intense flu activity, according to the CDC.
Overall flu activity has increased across North America this year with detections of predominantly influenza A H3N2 viruses, according to the World Health Organization's latest influenza update. In Europe, influenza activity increased above baseline levels in most countries in Northern and Southwestern Europe, according to WHO. In those regions, influenza B virus detections were frequent.
Flu vaccines typically provide better protection against influenza B or influenza A H1N1 viruses than against influenza A H3N2 viruses, according to CDC.
Major limitations of the new study include that it was conducted only in mice and ferrets, and that experiments were performed only on the influenza A virus.
"We need to perform a similar study on influenza B virus, which also causes flu," Sun said.
Mutant virus built vaccine
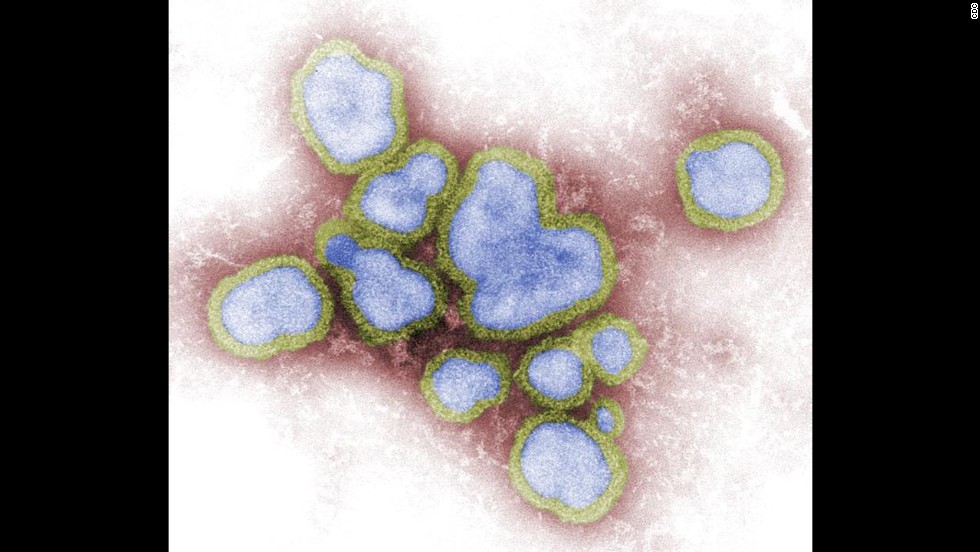
The new study involved an influenza A H1N1 virus that the researchers genetically engineered to incorporate certain mutations that made the virus hypersensitive to interferons, proteins involved in alerting the immune system to viral infections.
The researchers then measured how the virus behaved in mice and ferrets, the most commonly used animal models for influenza studies. The animals were vaccinated through the nose with a wild-type flu virus or the mutant virus at different doses.
The researchers found that their newly developed virus acted like a highly attenuated vaccine in the animals and produced higher interferon production than the wild-type flu virus.
In other words, by investigating the whole viral genome and introducing mutations that made the virus sensitive to interferons -- a first line of defense against viral infections -- the researchers used a radical approach to then develop a vaccine that gave interferons a big boost.
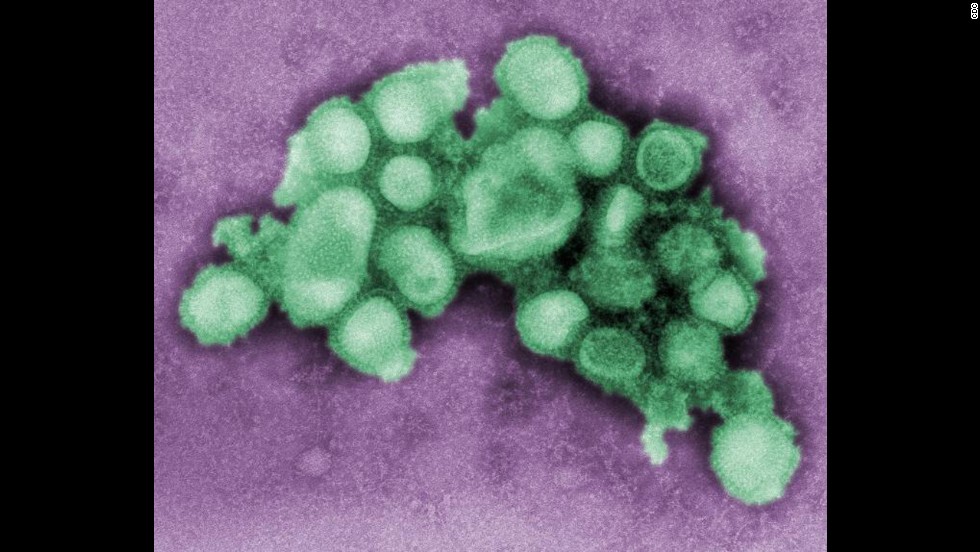
Attenuated or live vaccines use a weakened form of a germ, such as the new study's mutant virus, to prevent infections. Since these attenuated vaccines are so similar to a natural infection, just one or two doses could give you a lifetime of protection, according to the US Department of Health and Human Services.
Live vaccines have some limitations. Because they contain a small amount of the weakened live virus, they might not be safe for people with weakened immune systems, long-term health problems or individuals who've had an organ transplant. Live vaccines also need to be kept cool, so they don't travel well, which means they can't be used in regions with limited access to refrigerators, for instance.
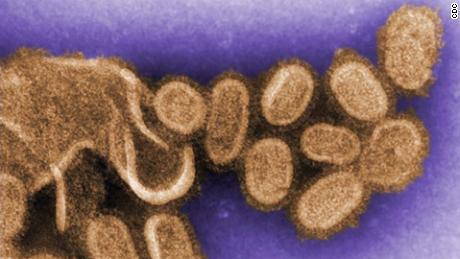
Typically, inactivated vaccines are used to protect against the flu. Such vaccines involve the killed version of a virus and usually don't provide immunity that's as strong as live vaccines, which is why in some cases you may need several doses over time, such as booster shots.
"The conventional approach to developing flu vaccines today is one in which we perform surveillance worldwide," said David Topham, director of the New York Influenza Center of Excellence and professor of microbiology and immunology at the University of Rochester in New York.
"We collect the viruses that are circulating in people," said Topham, who was not involved in the new study. Those viruses then typically are studied in ferrets, he said.
"We create an antigenic map of each virus and determine how similar or different that is than the (current) vaccine strain, and if it's different enough from the vaccine strain then we select that virus to be in next year's vaccine," Topham said. In other words, they make their best guess on what strains will be most likely to spread and cause illness based on surveillance data.
On the other hand, the new study suggests "using high-throughput sequencing methods and genetic engineering to rationally design a virus to use as a vaccine," he said. "I thought it was a very innovative and comprehensive approach."
The new study acted like "rocket science" compared with the conventional approach used to develop flu vaccines, he said.
The search for a universal flu vaccine
So what does the future hold for flu vaccines and where could this new approach fit in? There has been a shift among researchers around the world to focus on developing universal vaccines, Topham said.
"These, for influenza, would be vaccines that would last for at least five years and protect against 75% of the viruses that are out there," he said. "There are many ways that we might be able to achieve that. This approach that's described in this paper is just one approach."
The National Institutes of Health's National Institute of Allergy and Infectious Diseases influenza research program has focused on just that. It is working to develop a universal flu vaccine, which the program describes as a vaccine that provides robust, long-lasting protection against multiple subtypes of flu, rather than a select few.
The hope is that a universal vaccine could eliminate the need to update and administer the seasonal flu vaccine each year and could provide protection against newly emerging flu strains, potentially even those that could cause a flu pandemic.
In October, a separate group of researchers in the United Kingdom announced plans to begin "widespread human testing" of what it called a "universal flu vaccine" in adults 65 and older. They hoped to enroll 2,000 patients in the trial to determine effectiveness.
In an editorial accompanying the new study in the journal Science, authors John Teijaro, an assistant professor at the Scripps Research Institute, and Dennis Burton, a professor of immunology and microbiology at the institute, wrote that the "holy grail" of the influenza virus vaccine field is a universal vaccine.
They added that the new study "may be a step toward a universal influenza vaccine."
"However, many challenges remain," they wrote. "Data on cross-protection are limited to exposure to a small set of strains from the H1N1 and H3N2 subtypes of influenza viruses. It would be valuable to test additional viruses, including highly virulent avian subtypes such as H5N1 and H7N9, during subsequent challenge studies."