Story highlights
Antimicrobial resistance is one of the greatest threats to global health
193 counties signed a declaration to combat the problem at the UN General Assembly
Global leaders met at the United Nationals General Assembly in New York Wednesday to address what experts are calling one of the biggest threats to global health: antimicrobial resistance.
It is only the fourth time in UN history that a health issue has been discussed at the assembly, after HIV, noncommunicable diseases such as obesity, and Ebola.
The high-level meeting on antimicrobial resistance saw heads of statecommit to address the issue, with 193 countries signing a landmark declaration that they will combat resistance and rid the world of “superbugs.”
Drug-resistant bacteria are expected to kill 10 million people a year by 2050 – that’s one person every three seconds – if nothing is done to solve the problem.
Here are five things you need to know about antimicrobial resistance.
1. What is antimicrobial resistance?
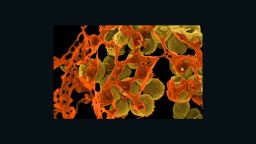
Antimicrobial resistance, commonly called AMR, is when bacteria, viruses, fungi and parasites become resistant to the drugs typically used to treat people infected by them. The drugs, which previously would have cured people of an infection, are no longer effective in killing the microbes. These resistant infections are often called superbugs.
“There are now many infections that cannot be treated at all,” said Dr. Vicky Enne, a clinical microbiologist at University College London who is working on new diagnostics to better target prescriptions. “And the problem is becoming worse as the (microbes) are becoming more and more resistant.”
Drugs once used to treat infections no longer work on a group of bacteria called Carbapenem-resistant enterobacteriaceae (CPE), which include common bacteria such as E. coli and Klebsiella pneumoniae. Others include methicillin-resistant staphylococcus aureus (MRSA), pseudomonas aeruginosa – typically acquired in hospitals – and gonorrhea. Enne notes that these infections can become severe if left untreated, leading to pneumonia, urinary tract infections, sepsis and death.
Infections such as HIV, tuberculosis and malaria are becoming increasingly untreatable because of antimicrobial resistance. Some infections require the use of older, more toxic antimicrobials as a last resort, but they’re sometimes developing resistance even those drugs.
“It basically compromises the whole of modern medicine,” she said.
2. Who is at risk?
Experts warn that everyone will be affected if nothing is done to address resistance as soon as possible.
Treating cuts and wounds could become problematic due to the risk of untreatable infection, and easy-to-cure infections such as gonorrhea will be rendered untreatable.
Childbirth and procedures such as cesarean sections, organ transplants, wound treatments and other forms of surgery will become high-risk as doctors lose access to antimicrobials that would normally protect patients from infection on the operating table.
The world will move back to a pre-antibiotic era, warned Enne.
For the moment, however, the people at most risk are those in the hospital, particularly those who are immunocompromised, such as chemotherapy patients, and are more likely to pick up one of these infections.
Another group at greater risk is residents of less-developed countries or countries with weaker health systems, as resistance is being reported in these regions more regularly. Enne highlights Asia and Southern Europe as places where untreatable cases have been reported, but adds that data are insufficient on the current situation in African countries.
For those in the West, infections can mostly still be treated in some way, but options are fast running out.
“If not action is taken, we’ll see serious problems by the time our children grow up,” said Enne.
3. Why has resistance developed?
There are many reasons underlying why resistance has emerged so widely among infectious microbes.
Some resistance happens naturally, due to underlying biology. The rapid replication rates of bacteria, viruses, parasites and fungi mean their turnover is high, and they are able to quickly evolve past a problem they encounter, such as a drug that is trying to kill them. The microbes that mutate and develop resistance to a drug will be the ones that survive and go on to proliferate the most.
But human behaviors and practices have helped these microbes evolve faster and more strategically than they otherwise may have, namely the widespread use of antimicrobials, offering more opportunity for the bugs to become resistant.
Among the problems: Antimicrobials are overprescribed and people buy them over the counter in certain countries. Drugs are shared, people don’t finish courses of treatment and antibiotics are overused in veterinary practices. Another large-scale use of antimicrobials – mostly antibiotics – has been in farming, to promote animal growth. This is still standard practice in the United States and many parts of the world except the European Union, where these practices are banned.
Essentially, the widespread use of antibiotics – in both humans and animals – has helped microbes evolve to become resistant.
4. What can be done?
Enne says it’s not too late to reduce the amount of resistance if individuals and governments alike commit to tackling the problem. “A lot of people aren’t aware of the seriousness of it all,” she said.
New antibiotics are needed to take the place of those that have been made redundant, but experts warn that this can take decades, so amending current practices is an immediate priority.
What can individuals do? Wash your hands more regularly to avoid both contracting and spreading infections, especially when visiting people in the hospital.
You can also spread the word and help others become more aware. Ensure that you finish any course of antimicrobials prescribed to you, avoid sharing any drugs prescribed to you or buying any over the counter, and try to buy meat from farms that do not use antibiotics on their animals.
Also, if your physician doesn’t think you need antibiotics, you probably don’t. So just accept it. “People can help by not pressurizing their general practitioners for antibiotics,” Enne said.
On a much larger scale, the solution will have to come from world leaders committing to end the problem, as they just have at the UN General Assembly, and creating policies and funds that support solutions.
The final report (PDF) from the Review on Antimicrobial Resistance, published in May, set out 10 recommendations to tackle resistance on a global scale by reducing unnecessary use, with a particular focus on four items: a global public awareness campaign, the supply of new antibiotics through increased research and development, improved diagnostic tests to ensure that antimicrobials are used only when needed, and reducing the unnecessary use of antibiotics in agriculture.
But all of this needs commitment and investment, stressed Enne, which is the goal of today’s declaration.
“We’ve seen it addressed in various global forums. Hopefully, there will be willingness and investment from around the world,” she said.
5. What are the consequences if nothing is done?
Today, superbugs are estimated to cause 700,000 deaths every year. If no action is taken as laid out, these numbers are expected to rise to 10 million deaths each year by 2050.
Follow CNN Health on Facebook and Twitter
In addition to a basic lack of treatment for infections, many medical procedures will not be possible, adding to the number of possible deaths.
“Doctors won’t be able to carry out life-saving procedures due to the risk of infection,” Enne said.
In a statement supporting today’s UN declaration, WHO Secretary-General Dr. Margaret Chan said, “antimicrobial resistance poses a fundamental threat to human health, development, and security.”
If nothing is done, the last drugs standing will be knocked out of the game, and modern medicine will not be so modern.
“Antibiotics underpin the whole of modern medicine,” Enne said, warning of the size of the challenge ahead. “It will be a considerable feat to solve the problem.”